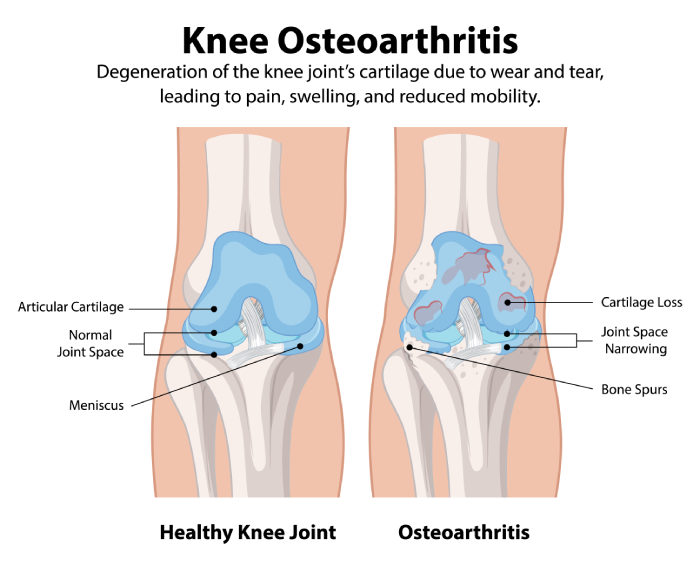
Exploring the Link Between Vitamin D Deficiency and Osteoarthritis Severity
Vitamin D is widely recognized for its critical role in maintaining musculoskeletal health. However, its specific impact on functional status in elderly individuals with osteoarthritis (OA), particularly knee OA, remains underexplored. This study delves into the association between vitamin D deficiency and functional impairment in OA patients, while also investigating potential correlations with inflammatory markers such as tumor necrosis factor alpha (TNF-α) and interleukin-6 (IL-6).
Study Design and Methodology
The research involved older adults aged 60 and above, drawn from an aging study cohort. The participant pool included 105 individuals diagnosed with OA and 152 controls. OA diagnosis was confirmed through radiographic imaging, and functional impairment was assessed using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaire. Blood samples were collected to measure serum levels of 25-hydroxyvitamin D [25(OH)D] using chemiluminescence, while TNF-α and IL-6 levels were quantified via enzyme-linked immunosorbent assay (ELISA).
Key Findings
1. Vitamin D Levels and OA Severity:
Patients with vitamin D insufficiency or deficiency exhibited more severe OA symptoms compared to those with normal vitamin D levels (p = 0.04). This suggests a potential protective role of adequate vitamin D levels in mitigating OA progression.
2. Functional Impairment:
Vitamin D levels were inversely correlated with functional impairment, as measured by the WOMAC Index. Specifically, global functional impairment (rS = −0.25, p = 0.01) and pain severity (rS = −0.21, p = 0.03) were significantly worse in patients with lower vitamin D levels.
3. Inflammatory Markers:
OA patients with vitamin D deficiency had significantly higher levels of TNF-α and IL-6 (p < 0.05, Mann−Whitney test). These findings indicate a potential link between vitamin D deficiency and increased systemic inflammation, which may exacerbate OA symptoms.
Implications of the Study
The study highlights a clear association between vitamin D deficiency and worsened OA outcomes, including greater functional impairment, increased pain, and elevated inflammatory markers. These results underscore the importance of maintaining adequate vitamin D levels, particularly in elderly populations at risk for OA.
However, the study also raises important questions about the mechanisms underlying these associations. Does vitamin D deficiency directly contribute to OA progression, or is it a marker of other underlying factors? Additionally, while the study suggests a potential benefit of vitamin D supplementation, further research is needed to determine whether supplementation can effectively reduce OA symptoms and slow disease progression.
Limitations and Future Directions
While the study provides valuable insights, it is not without limitations. The cross-sectional design limits the ability to establish causality, and the relatively small sample size may affect the generalizability of the findings. Future longitudinal studies with larger cohorts are needed to confirm these results and explore the potential therapeutic benefits of vitamin D supplementation in OA patients.
Commentary by SuppBase columnist Alice Winters
This study offers a compelling exploration of the relationship between vitamin D deficiency and osteoarthritis, particularly in elderly populations. The findings align with existing research that underscores the importance of vitamin D in musculoskeletal health, but they also break new ground by linking vitamin D levels to functional impairment and systemic inflammation in OA patients.
From a nutritional science perspective, the inverse correlation between vitamin D levels and WOMAC scores is particularly noteworthy. It suggests that maintaining optimal vitamin D levels could play a role in preserving mobility and reducing pain in OA patients. However, it is important to approach these findings with caution. While the study identifies a correlation, it does not establish causation. Factors such as reduced outdoor activity (which affects vitamin D synthesis) or comorbid conditions could also contribute to both vitamin D deficiency and OA severity.
The elevated levels of TNF-α and IL-6 in vitamin D-deficient patients add another layer of complexity. These inflammatory markers are known to play a role in joint degradation and pain, and their association with vitamin D deficiency raises intriguing questions about the interplay between nutrition and inflammation in OA. Could vitamin D supplementation help modulate these inflammatory pathways? While the study does not answer this question directly, it provides a strong rationale for further investigation.
From a consumer perspective, this study highlights the potential benefits of vitamin D supplementation, particularly for older adults at risk for OA. However, it is crucial to emphasize that supplementation should be approached thoughtfully. Excessive vitamin D intake can lead to toxicity, and individual needs vary based on factors such as sun exposure, diet, and baseline vitamin D levels. Consulting a healthcare provider before starting any supplementation regimen is essential.
In conclusion, this study adds valuable insights to the growing body of evidence supporting the role of vitamin D in musculoskeletal health. It also underscores the need for further research to fully understand the mechanisms at play and to evaluate the potential benefits of vitamin D supplementation in managing OA. For now, maintaining adequate vitamin D levels through a balanced diet, sensible sun exposure, and, if necessary, supplementation remains a prudent strategy for supporting overall health and potentially mitigating OA symptoms.